Advances in Battery Technology Enabling Implanted Sensors in Next-Generation Medical Devices
Posted on: in Blog
As medical devices and implants continue to advance it was only a matter of time before they evolved to provide real-time data back to medical staff and patients. A key challenge has been ensuring that the implanted sensors that wirelessly relay this data back have the right battery power. With the right power, these devices can start to cover more health conditions such as :
- Chronic pain, traditionally treated with medicine has suffered misuse which led to the increasing opioid crisis, in particular in the US. Implanted neurostimulation devices are seen as safe, long term replacement
- Sleep Apnoea where an implantable device can stimulate key airway muscles to stay open and sensors can feed back data about the condition
- Implantable pulse generators (IPG) which are neurostimulators
- Heart conditions currently treated with cardiac pacemakers or defibrillators that support heart rhythm management. Implanted sensors can monitor data such as progression of heart failure and success of new treatment. Blood pressure devices that monitor blood pressure, giving early warning of a possible heart attack
- Eye implants, either for the correction of sight or intra-ocular pressure (which if high can lead to glaucoma), or for real-time glucose monitoring to help diabetics manage their condition
- Smart implants such as next-generation prosthetic implants (knee, shoulder, hip) to monitor performance, signs of infection or malfunction, pressure and temperature.
Current sensors are placed outside the body but can be bulky and don’t always give accurate data. Implanted sensors can give much more reliable data on a regular basis as they are embedded inside the actual implant.
By sending data back to the medical team, they provide an early warning signal so action can be taken, preventing any further damage. In smart orthopaedics for example, one frequent problem is when muscle and tissue react to the foreign material of the implant and this only comes to light when something goes wrong with the implant, or the patient suffers pain. An implanted sensor will feed back data so intervention can take place. This sort of intervention can:
- Have huge cost savings for healthcare providers
- Reduce recovery time for the patient
- Prevent secondary injuries
- Increase the life span of implant
- Inform treatment plans
Real-time data won’t just help doctors but also those designers of future medical devices, giving them more data to create even better implants. To date, a key challenge has been to make the sensor small enough to fit into these next-generation implants. The use of microelectromechanical systems (MEMS) based technology has made this possible. However battery technology has also needed to improve to be small enough to fit inside these microscale sensors.
Ilika’s Stereax solid state batteries are designed to address the challenges designers face with next-generation medical implants. These micro batteries:
- Are ultra-thin down to 150 µm
- Have no toxic liquids
- Can be as small as 2 mm3
- Support high temperatures
- Are customisable in shape and form
- Have high energy and can be stacked to increase energy
- Can be powered wirelessly
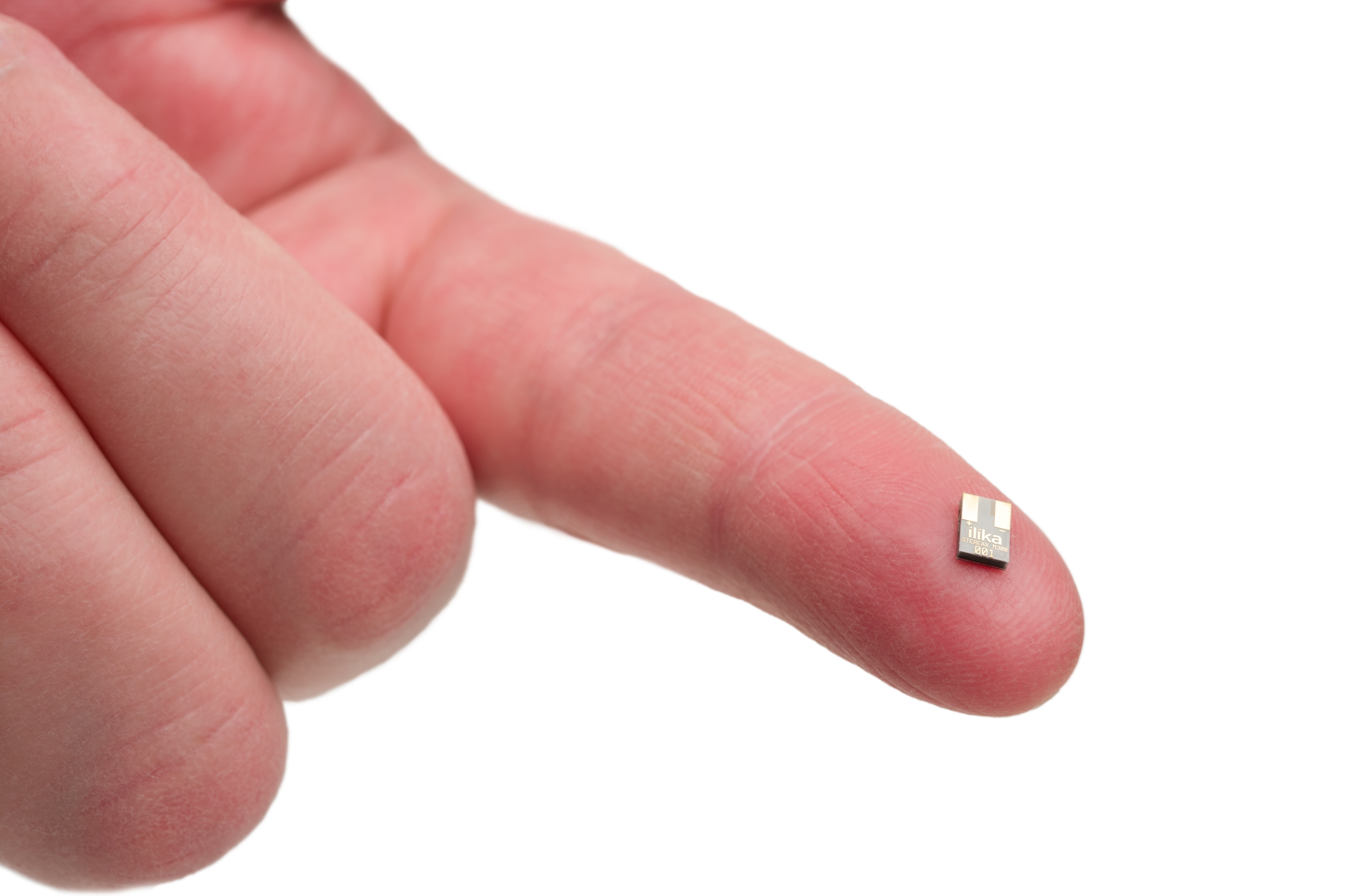
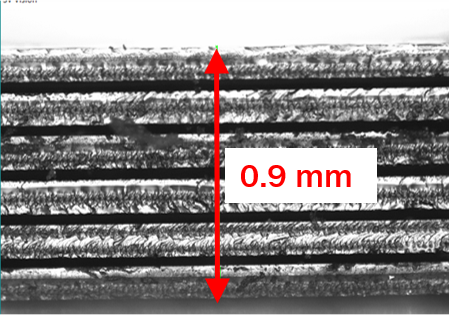
The Stereax M300 - a miniature stacked battery. It will have a capacity of 300 µAh and dimensions of 5.6 mm x 3.6 mm x 0.9 mm. We do this by dicing, thinning and stacking 6 cells in less than 1 mm thickness.
We’re currently working with product designers to develop customised batteries for their smart implants enabling them to innovate as much as possible and not be limited by the battery power. Engage now as an early adopter info@ilika.com.
